Comprehensive Claims Processing & Administrative Solutions
Technology and expertise should not be obstacles but accelerators for your business success. You need solutions that adapt to your unique challenges and scale with your growth.
HealthAxis meets these demands with a suite of services, including our proprietary CAPS technology, BPaaS, BPO, staff augmentation, and consulting. Designed for efficiency and effectiveness, our solutions simplify health plan management, allowing you to concentrate on supporting your members’ healthcare needs.
Scaling Success with Customized Operational Support
Our expertise in tailoring services and technologies ensures:
Streamlined Operations
Optimized Costs
Improved Trust & Compliance
Elevated Member Experience

Why Partner With HealthAxis?
Scalability & Flexibility
Adapt and grow with our scalable technology & services, designed to evolve seamlessly with your business needs.
Integrated Excellence
Benefit from a holistic approach that ensures seamless coordination across all aspects of your health plan management.
Expert Assurance
Depend on our comprehensive expertise to guide you through industry complexities, delivering accuracy, compliance, and innovation.
Operational Agility
Achieve greater operational flexibility and cost efficiency with our combined services, designed to streamline your processes and support your strategic goals.
Optimize Your Health Plan Workforce with Precision
Feeling overwhelmed by the demands of your healthcare payer operations? We understand the challenges of staying ahead in a rapidly evolving industry. At HealthAxis, we recognize the stress of managing fluctuating workloads, meeting compliance standards, and sustaining quality member services.
With HealthAxis’s staff augmentation services, you’re not just filling positions; you’re enhancing your team’s capabilities. Our solution offers access to over 130 operational roles, each designed to boost efficiency and effectiveness in your organization.
Latest News and Insights
Stay up to date with the latest healthcare trends and grow your business.
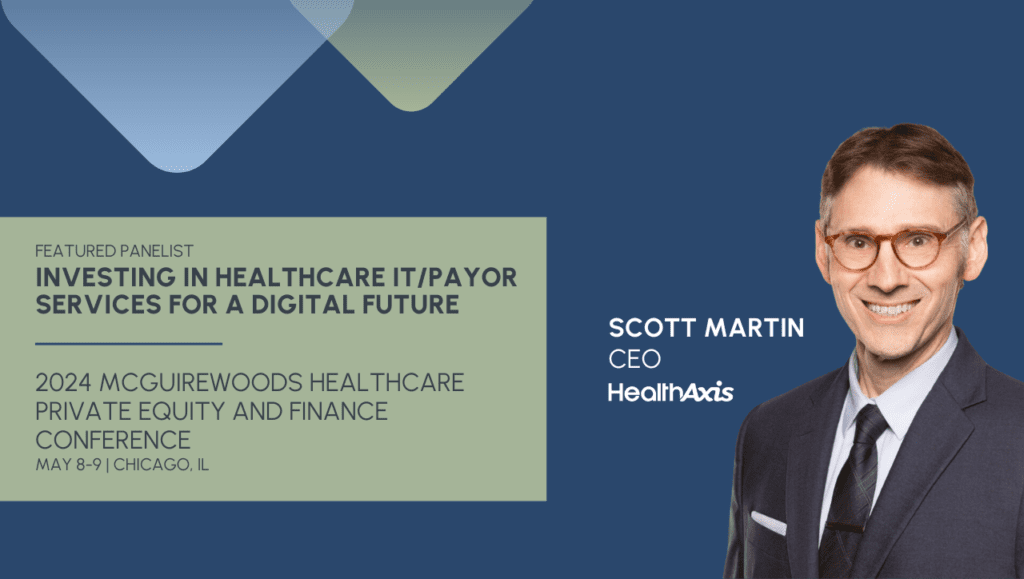
News
HealthAxis CEO Scott Martin to Speak at the 2024 McGuireWoods Healthcare Private Equity and Finance Conference
Social
HealthAxis by the Numbers
0+
Years of Experience$0B+
Claims Paid Annually0M+
Claims Processed Annually0+
Health Plans Served0+
Benefits Plans ManagedSee What Our Clients Are Saying
Ready To Transform Your Organization?
Schedule a Discovery Call
We'll discuss challenges with your current system, the services you need and your timeline.
Receive a Personalized Demo
Our team will demonstrate how you can automate tasks and integrate with existing programs.
Experience a Fast & Professional Implementation
With your dedicated customer service team, the process is seamless.
Get Unmatched Support, Training and Expertise
With more than 55 years in the industry, we know what works.